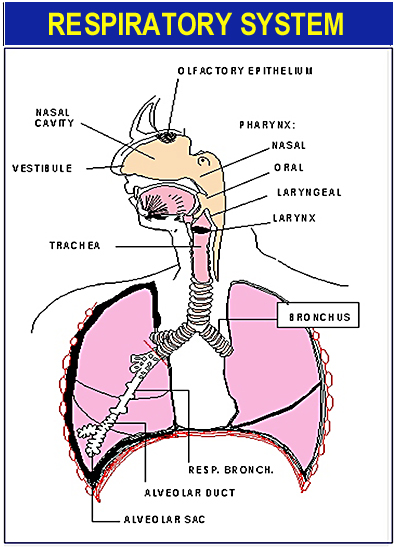
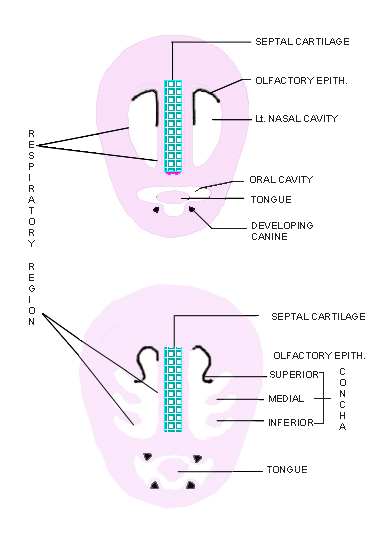
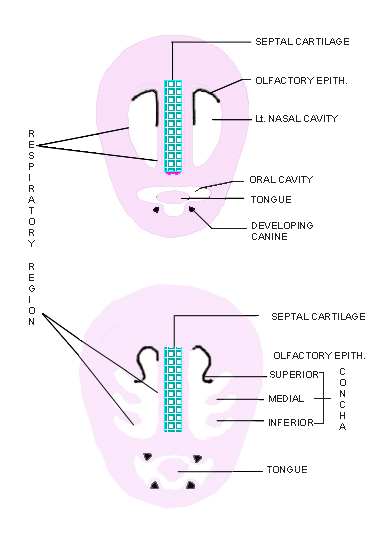
1. The vestibule -- opens to the outside at the
anterior nares. The integument continues into the
vestibule; Changes from cornified stratified squamous epithelium (associated
with hairs, sebaceous and sweat glands) gradually to pseudostratified,
ciliated, columnar epithelium in the rest of the nasal cavities (i.e.
atrium, superior-, middle-, and inferior meatus; the surface of conchae).
2. The respiratory region -- includes nearly all
of the septum and lateral walls. The surface area of the lateral walls
is increased by shelf-like projections (supported by bone) called
conchae (Figure 3).
|
a. Epithelium: pseudostratified, ciliated columnar
with goblet cells; Cilia beatsbackwards, toward the pharynx; Goblet
cells sometimes are concentrated in intraepithelial pits; The basement
membrane varies from thin to very thick.
|
b. Lamina propria: of
loose FECT;
i. contains: mixed sero-mucous glands (comp. tubuloalveolar);
ii. contains: a rich cavernous venous plexus, which serves to
warm the passing air; upon irritation the plexus can be distended
by blood and reduces air flow.
c. Submucosa:
lacking, the deepest layer of the lamina propria fuses with the
periosteum below;
|
3. The olfactory region -- located on the superior
concha and adjacent septum (dime-size areas).
a. Epithelium: pseudostratified ciliated
columnar; composed of olfactory cells, supporting cells,
and basal cells. (Figure 4).
|
C. THE PHARYNX -- is a flattened conical chamber through
which air and food pass. It is divided partly by the soft palate into:
|
1. Naso-pharynx -- lined with ciliated
columnar epithelium with goblets cells;
|
2. Oro-pharynx -- lined with moist
stratified squamous epithelium.
|
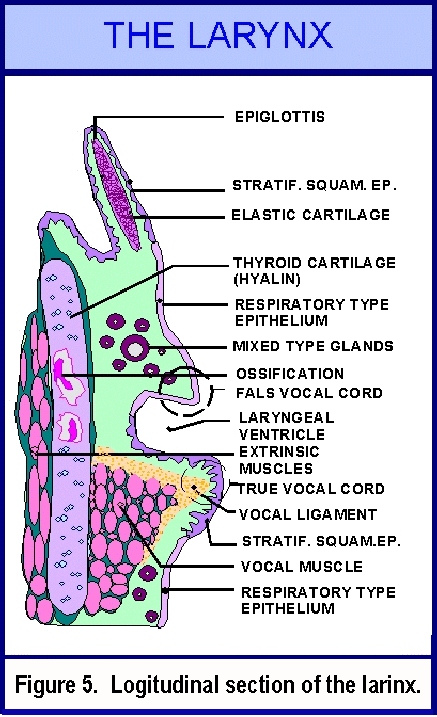
D. THE LARYNX -- is interposed between the pharynx
and the trachea. It is supported by cartilages and muscles; and contains
the vocal folds (cords). Figure 5.
|
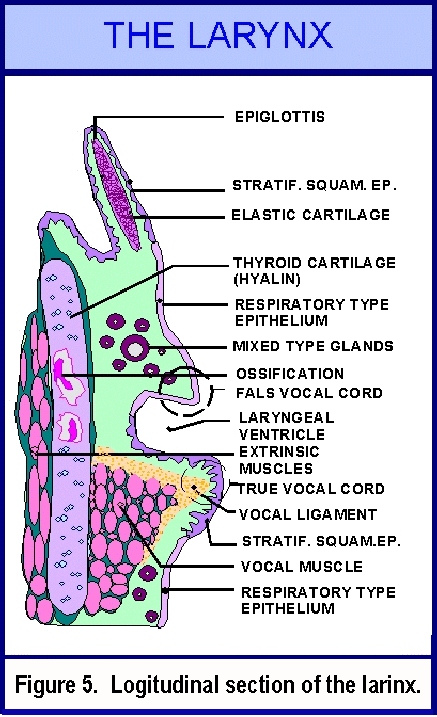 |
1. Epithelium -- varies according
to wear and tear in the different regions of the larynx. |
a. The epiglottis -- which closes that laryngeal aperture
like a lid, is covered by moist stratified squamous epithelium;
|
b. The false vocal cords - (located above the true
vocal cords) are covered with pseudostratified, ciliated
columnar epithelium with goblet cells.
|
c. The true vocal cords - are covered with moist stratified
squamous epithelium.
|
d. The rest of the larynx is covered with pseudostratified,
ciliated columnar epithelium with goblet
cells (including the lateral walls of the laryngeal ventricles between
the false and true vocal cords), resting on a thin
basement membrane. The cilia beat toward the mouth, moving the mucus
and attached particles or bacteria toward the exterior.
|
| |
2. Lamina propria -- is rich in elastic
fibers. |
| |
|
a. In the true vocal cord there is an elastic
band that constitutes the vocal ligament and it is adjacent
and parallel to the vocal muscle in the deeper layers of
the lamina propria. |
| |
|
|
| |
|
b. The glands in the larynx are tubuloacinar,
mixed (sero-) mucous glands, they are absent from the avascular vocal cords. |
| |
|
| |
3. Cartilages -- support the walls
of the larynx; |
| |
|
They are united by ligaments and maintain the larynx as a
constantly open tube. Early in life all are of the hyalin
type. Latter most of the epiglottis and arytenoid
cartilages become elastic and smaller parts of these may
become fibrocartilage. In sum, the larger cartilages remain
hyalin (e.g., thyroid cart.) while the small ones become
elastic. |
| |
|
|
| |
4. Functional correlations: |
| |
|
| |
|
a. The extrinsic muscles of the larynx -- muscles which
attach to the cartilages externally -- aid in swallowing (deglutition);
|
| |
|
|
| |
|
b. The intrinsic muscles -- muscles which
interconnect the cartilages -- function in changing the pitch of the sound
(e.g. vocal muscle); |
| |
|
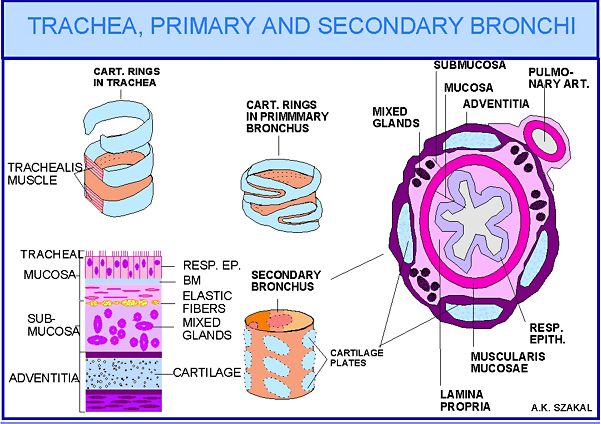
E. TRACHEA, PRIMARY AND SECONDARY BRONCHI -- thin walled, flexible,
extensible tubes.
|
| |
The trachea is supported by C-shaped cartilages,
with the open part of the C facing the esophagus and it is spanned by
the trachealis muscle and a membrane of D.-FECT. Adjacent
cartilages are connected by dense fibro-elastic membranes.
The trachea (4.5 inches long and 1 inch in diameter)
bifurcates and gives rise to the primary (or main) bronchi which are held
open by rings of hyalin cartilage.
|
| |
|
|
| |
|
1. Epithelium -- is of the respiratory type,
- pseudostratified, ciliated columnar with many goblet cells. It rests
upon a very prominent basal lamina (cilia move mucus
in an external direction).
|
| |
|
2. Lamina propria -- is a thin layer, with longitudinal
elastic fibers in place of muscularis mucosa in the trachea
and with muscularis mucosa (sm.m.) in
the bronchi. Reticular fibers are abundant below the basal lamina.
|
| |
|
3. Submucosa -- is a deeper layer
with tubuloacinar, mixed (sero-) mucous glands. |
| |
|
4. Adventitia -- is a dense irregular
connective tissue layer surrounding the trachea and the bronchi and contains
the cartilages. The cartilaginous rings of primary bronchi (Figure
6) are replaced by irregular cartilaginous plates in the adventitia,
after the bronchi enter the substance of the lungs; These bronchi with the
cartilaginous plates are the secondary bronchi. |
|
II. HISTOLOGY OF THE RESPIRATORY SYSTEM
|
The respiratory unit of the lung is the primary lobule
which consists of the:
|
| |
|
|
|
|
A. Respiratory bronchiole |
|
| |
|
|
|
|
B. Alveolar ducts |
|
| |
|
|
|
|
C. Alveolar sacks |
|
| |
|
|
|
|
D. Alveoli |
|
| |
|
|
|
|
E. Associated blood vessels, lymphatics, nerves, C.T.
|
|
|
|
|
Figure 7. Illustrates the microanatomy
of bronchioles and alveolar sacs.
|
A. RESPIRATORY BRONCHIOLE -- in adult man
they begin with a 0.5mm diameter. A few alveoli bud from their walls.
|
1. Epithelium -- starts with a simple ciliated
columnar epithelium which is reduced in a short distance to a simple
(non-ciliated) low cuboidal epithelium.
|
2. Wall -- composed of collagenous C.T.
interlaced with bundles of smooth muscle.
(The few alveoli associated with the wall are responsible for the
term "respiratory bronchiole.")
|
B. ALVEOLAR DUCTS -- are the branches (2 to 11)
of respiratory bronchioles. These are thin walled tubules. Their wall
is interrupted by the opening of many thin walled outpouchings, the
alveoli.
|
1. Epithelium -- not distinguishable.
|
2. Wall -- composed of strands of elastic and
collagenous fibers, and a few smooth muscle cells which are visible
around the mouth of alveolar sacks.
|
C. ALVEOLAR SACKS -- are composed of 2 to 4 or more
alveoli. Alveolar sacks open only into the alveolar
ducts. The space into which alveolar sacks open in the alveolar duct
is called the atrium.
|
D. THE ALVEOLUS -- is a thin walled polyhedral sack
which opens on one side only into the alveolar sack
or individually into an alveolar duct ( Figure 8.)
|
|
|
Figure 8. Shows the microanatomy of the alveolus.
|
| |
1. The walls of alveoli contain a dense network
of anastomosing capillaries; reticular fibers and elastic fibers
form the supporting framework of the wall. There are small openings
in the wall (alveolar septum) between adjacent
alveoli; these are called alveolar pores (7-9mm
diameter).
|
2. The epithelial lining of the alveolus:
|
a. it is of endodermal origin;
|
b. constitutes a thin cellular covering (clearly visible only
with the electron microscope); separated from the endothelium
of capillaries by a continuous basal lamina.
|
c. The cells composing this layer are:
|
i. the squamous pulmonary epithelial cells
(Type I pneumocytes);
|
ii. the rounded great alveolar cells (Type
II pneumocytes).
|
iii.Function: a. Type
II pneumocytes secrete pulmonary
surfactant (rich in phospholipids) in
the form of multilamellar bodies.
|
b. the faulty production or absence of surfactant
in newborns results in the fetal distress syndrome
(hyalin membrane disease).
|
c. Type I pneumocytes function as lining
cells of alveoli and thought to have the potential of differentiating
into Type II pneumocytes.
|
| |
3. Alveolar phagocytes (Pulmonary or lung macrophages,
also known as dust cells).
|
a. Originate from blood borne monocytes;
|
b. Migrate into interstitium (C.T.) of lung and from there into
the alveoli;
|
c. Similar to other macrophages;
|
d. Function in the removal of cell debris and foreign material
(e.g. dust) from the lung.
|
Blood supply of the lung: via large elastic pulmonary
arteries whose branches accompany the bronchi and its branches as far
as the respiratory bronchioles. Alveoli are supplied by capillaries
from branches at the level of the alveolar duct. Venules arise from
the alveolar septa and from the pleura, run independently
of arterioles and form the pulmonary veins which return
the blood to the heart. The bronchi are supplied with blood independently.
|
| |
The Pleura -- consists of a thin layer of collagenous
connective tissue interspersed with layers of elastic fibers, and a
layer of mesothelial cells. The visceral pleura covers
the surface of the lung and the parietal pleura forms
the lining of the thoracic cavity.
|
| |
***********************************************************************
LABORATORY EXERCISE:
Virtual Slide 74, Lung (
Bronchioles and alveoli).
Study the CD first then identify the same structures on the virtual
slide 74. Identify bronchioles, respiratory bronchioles, alveolar ducts,
alveolar sacs, and alveoli. What is the difference between terminal
and respiratory bronchioles? How can you distinguish alveolar ducts?
Identify Type I and Type II pneumocytes. Find and study the morphology
of alveolar macrophages and macrophages in the interstitium. Why are
pulmonary phagocytes (macrophages) sometimes called dust cells?
***********************************************************************
|
| |
| RESPIRATORY SYSTEM LAB REQUIREMENTS: |
| Structures to be identified: |
|
nasal septum
classify cartilage
identify perichondrium
identify conchae
Junction of respiratory and olfactory epithelium
classification of these epithelia
olfactory cells
supporting cells
basal cells
Bowman's glands
olfactory nerves
Identify and/or classify:
laryngeal and tracheal cartilages
false vocal fold
true vocal fold
laryngeal ventricle
classify epithelial covering of above
distribution of glands (i.e., in falls and true vocal folds)
vocal ligament (id and classify both)
vocalis muscle
classify cartilage in epiglottis and thyroid cartilage
Identify and/or classify:
Four layers of trachea (what are they?)
I. mucosa: 1. classify and identify epithelium, Goblet cells, basement
membrane; 2. lamina propria;
II. muscularis mucosae;
III. submucosa, classify the glands;
IV. adventitia, cartilage
Identify and/or classify:
secondary bronchi
mucosa
muscularis mucosae
submucosa
glands
adventitia
cartilaginous plates
ordinary bronchiole and its layers
terminal bronchiole
respiratory bronchiole
alveolar duct
alveolar sacs
alveolusalveolar wall and components under (oil) 100X objective.
Squamous alveolar epithelial cell or Type I ep. cell
Great alveolar cell or Type II ep. cell
capillaries
basement membranes
alveolar macrophages (dust cells, heart failure cells, why?)
|